- Examination of Neck Veins – Venous Pressure
- Examination of Neck Veins – Venous Waveforms
Terms ‘venous waveform’, ‘venous pulse’ and ‘venous pressure waveform’ are used interchangeably in this article. All are related to jugular veins.
History
In late 19th century Sir James Mackenzie was the first physician who described abnormalities of neck veins. He focused solely on venous waveforms and completely ignored venous pressure. Nevertheless, labels he used to describe components of venous pressure waveforms are still used today. In 1902 after years of studies he published ‘The study of the pulse, arterial, venous, and hepatic, and of the movements of the heart’, an unprecedented book about his findings.
First he used simple sphygmograph to detect venous pulse that he later upgraded to polygraph to simultaneously measure arterial and venous pulse. It allowed him to study waveform abnormalities in cardiac arrhythmias and heart diseases before the era of electrocardiography.

A 35 year old female presents with shortness of breath on exertion. She denies any chest pain, cough, sputum or fevers. Her past medical history is significant for severe pulmonary hypertension. On physical examination her blood pressure is 135/75 mmHg. Heart rate is 110/min and regular. Her neck veins are visible and distended even in upright position.
Next you focus on venous waveform, looking for any abnormality possibly consistent with tricuspid regurgitation.
Physical Examination
- Setup. Have the patient lying supine on the bed, relaxed. Head of the bed can be elevated to 30° although adjustments (to more supine or upright) may be needed later on. The room should be well lit.
- Expose the neck. Ask the patient to turn head to the left so the right side of the neck is exposed. However, venous pulsations can be visualised on both sides.
- Identify pulsation. First try to identify any pulsation, then try to differentiate whether it’s arterial or venous. Venous pulsation has downward trend, have two pulsations per systole and changes with abdominal pressure or positioning of the patient. Arterial has upward movement, is easy palpable and does not change with pressure or position. Other characteristics are shown in a table below.
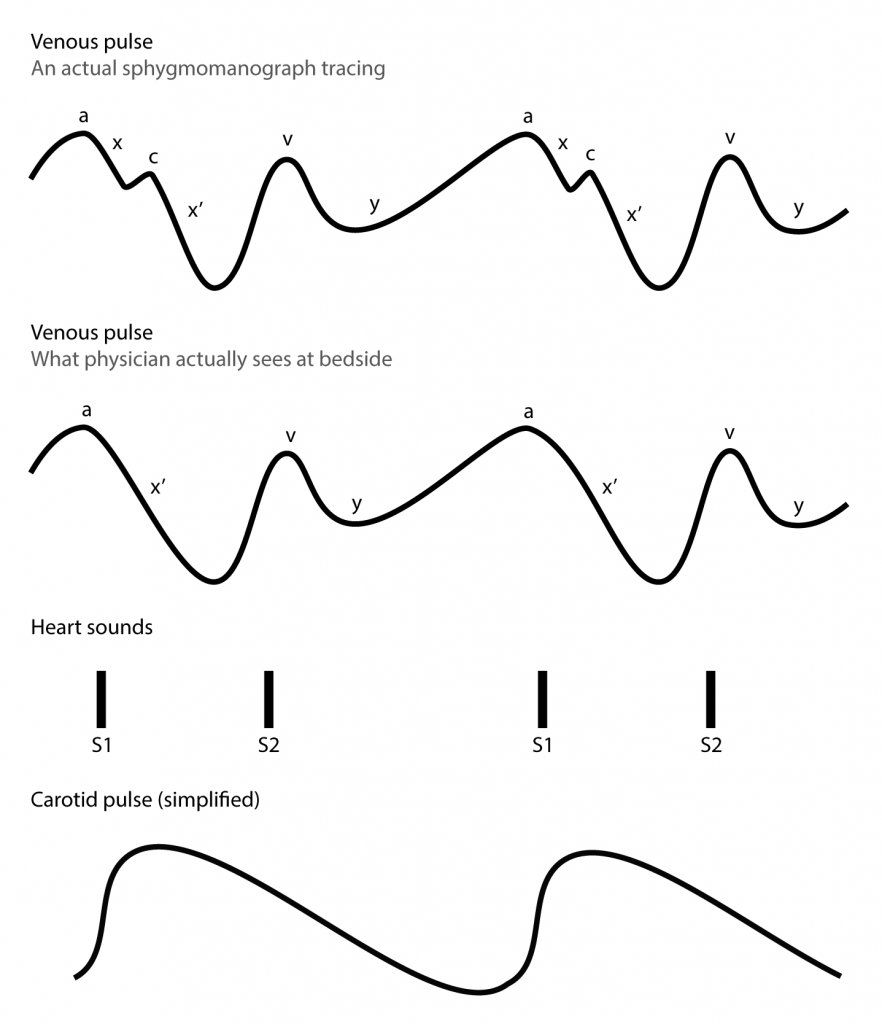
- Identify venous waveform. There are two ways how to identify venous pressure waveforms. On examination at bedside usually only venous pressure descents are easily visible. See illustration below.
- The easiest way is to listen to the heart sounds with stethoscope. x and x’ descend occur after S1 and ends just before S2. y descent begins shortly after S2. Similarly a wave begins just before S1 and v wave shortly after S2.
- Another possibility is to observe upstroke of carotid artery. x’ descent coincides with systolic carotid upstroke.
| Venous pulsations | Arterial pulsations | |
| Character of movement | Descending and inward | Ascending and outward |
| Palpability | Barely or not palpable | Easily palpable |
| Occludability | Easily occludable by light touch | Occludable only with hard pressure |
| Number of pulsations per cardiac cycle | Two | One |
| Change with respiration | Decrease during inspiration; increase during expiration | Does not change |
| Change with abdominal pressure | Temporarily increase during pressure | Does not change |
| Change with position | Increase with lowering the patient, decrease with sitting the patient up | Does not change |
Interpretation
Normal jugular venous pressure waveform has three upward deflections (waves) and three downward deflections (descents). However, on bedside examination only two descents are usually seen and there should be no outward movement.
a wave. Represents right atrial contraction. It’s not visible in atrial fibrillation. The end of a wave occurs simultaneously with carotid artery upstroke.
x descent. Represents right atrial relaxation and rapid atrial filling.
c wave. Corresponds to right ventricular contraction and bulging of the tricuspid valve. Normally, it’s not visible on bedside examination. The wave was originally named and mistaken by Mackenzie for carotid artifact.
x’ descent. Represents right ventricular systole and right atrial relaxation. Occurs when the tricuspid valve (base of the right atrium) moves down while the right ventricle contracts. The x’ descent can be used as a measure of right ventricular contractility.
v wave. Corresponds to right atrial filling, or venous filling when tricuspid valve is closed and venous pressure is rising. However it is important to note that most of the atrial filling occurs during ventricular systole.
y descent. Represents emptying of the right atrium into the ventricle following opening of the tricuspid valve.
An ‘old-but-gold’ film from 1957 explaining examination of jugular venous pulse is available.
Venous waveform abnormalities
To be added at later date.
Caveats and Errors
Patient position. Patient should be positioned to whatever level top of neck veins is best visualised. It may be supine, semi-upright in 30 or 45 degrees or even upright.
Visualising internal jugular vein. It’s important to understand that internal jugular vein lies underneath sternocleidomastoid muscle and is not that clearly evident to the external observation. It does not resemble subcutaneous vein and is frequently misidentified with external jugular vein by inexperienced observer. The pulsation is not clearly visible and has characteristic descending movement.
Clinical Significance
To be added at later date.
References
Chi, J., Artandi, M., Kugler, J., Ozdalga, E., Hosamani, P., Koehler, E., … Verghese, A. (2016). The Five-Minute Moment. The American Journal of Medicine, 129(8), 792–795. https://doi.org/10.1016/j.amjmed.2016.02.020
McGee, S. R. (2018). Evidence-based physical diagnosis (4th edition). Philadelphia, PA: Elsevier.
McGee, S. R. (1998). Physical examination of venous pressure: A critical review. American Heart Journal, 136(1), 10–18. https://doi.org/10.1016/S0002-8703(98)70175-9
Neck Veins & Wave Forms | Stanford Medicine 25 | Stanford Medicine. (n.d.). Retrieved 6 June 2018, from https://stanfordmedicine25.stanford.edu/the25/nvwf.html
James Mackenzie (cardiologist). (2018, April 17). In Wikipedia. Retrieved from https://en.wikipedia.org/w/index.php?title=James_Mackenzie_(cardiologist)&oldid=836907529
Jugular venous pressure. (2018, June 9). In Wikipedia. Retrieved from https://en.wikipedia.org/w/index.php?title=Jugular_venous_pressure&oldid=845167139